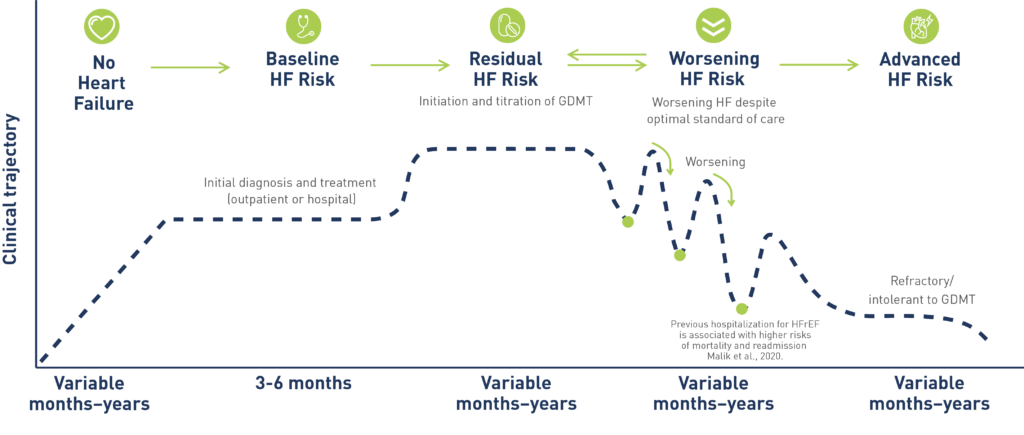
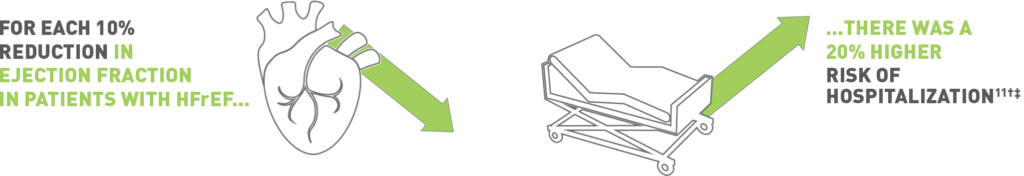
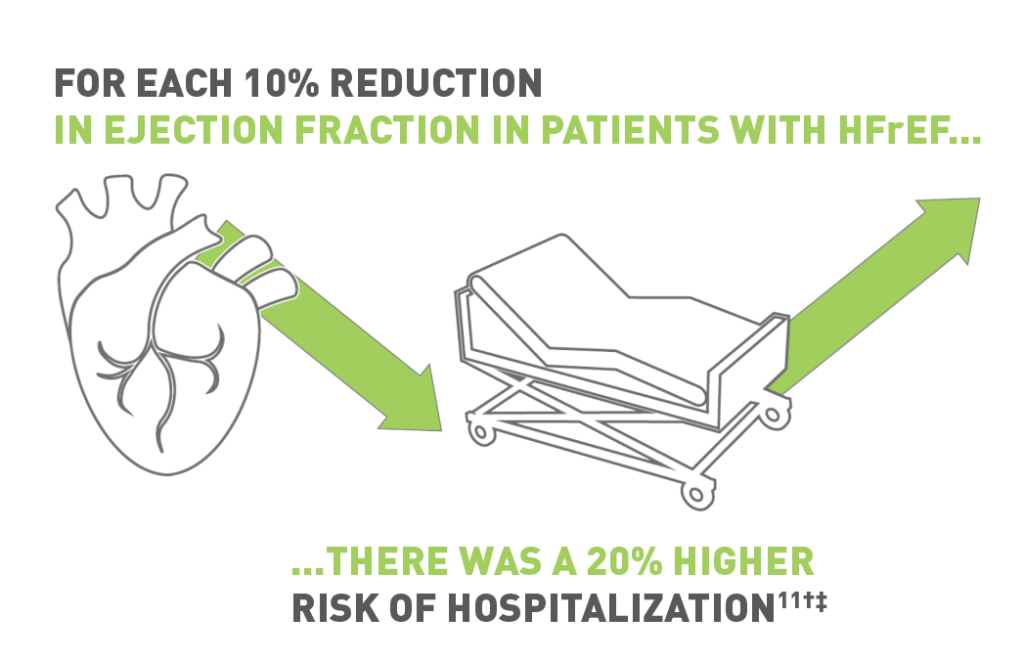
Left ventricular ejection fraction (LVEF) is an important prognostic factor when examining patients with worsening heart failure
- HFrEF is defined as LVEF ≤40% by 2022 AHA/ACC/HFSA heart failure guidelines7
For US Healthcare Professionals only
†Proportion of patients with cardiovascular death or heart failure hospitalization is aggregate data from the CHARM Program (CHARM-Alternative, CHARM-Added, and CHARM-Preserved pivotal trials) evaluating the efficacy and safety of candesartan in patients with New York Heart Association Class II to IV heart failure.2 Because the CHARM Program predates newer therapies for the treatment of HFrEF (eg, SGLT2i, ARNi), current rates for cardiovascular death or heart failure hospitalization may vary.
ACC, American College of Cardiology; AHA, American Heart Association; ARNi, angiotensin receptor neprilysin inhibitor; CHARM, Candesartan in Heart failure: Assessment of Reduction in Mortality; EF, ejection fraction; GDMT, guideline-directed medical therapy; HF, heart failure; HFSA, Heart Failure Society of America; NT-proBNP, N-terminal pro-brain natriuretic peptide; QoL, quality of life; SGLT2i, Sodium/glucose cotransporter-2 inhibitors.
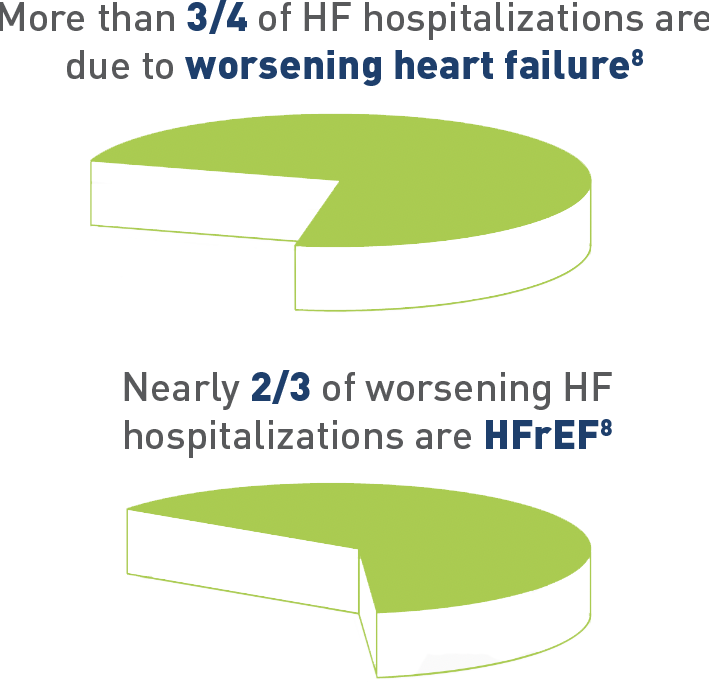
References: 1. Fonarow GC et al. J Am Coll Cardiol. 2007;50(8):768-777. 2. Tsao CW et al. Circ. 2022;145:e153–e639. 3. Butler J et al. J Am Coll Cardiol. 2019;73(8):935-944. 4. Gheorghiade M et al. Am J Cardiol. 2005;96(6A):11G-17G. 5. Greene et al. Eur J Heart Fail. 2019;21(1)121-124. 6. Malik A et al. Am J Med. 2020;133(1):84-94. 7. Heidenreich PA et al. J Am Coll Cardiol. 2022;79(17):e263-e421. 8. Chang PP et al. Am J Cardiol. 2014;113(3):504-510. 9. Setoguchi S et al. Am Heart J. 2007;154(2):260-266. 10. Rethy L et al. 2020;13(11):e007014. 11. Solomon SD et al. Circ. 2005;112(24):3738-3744. 12. Rørth R et al. Circ Heart Fail. 2020;13(2):e006541. 13. Okuhara Y et al. Sci Rep. 2019;9(1):17271. 14. Ito S et al. JACC Cardiovasc Imaging. 2020;13(2):357-369. 15. Huusko J et al. ESC Heart Failure. 2020;7:2406–2417. 16. Urbich M et al. PharmacoEconomics. 2020;38(11):1219-1236. 17. de Almeida FA et al. Health Qual Life Outcomes. 2020;18(262):1-10. 18. Dunbar SB et al. J Card Fail. 2021;27(8):877-887.
